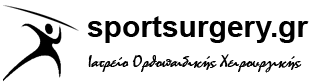
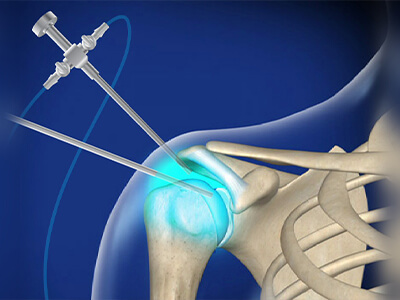
ΑΡΘΡΟΣΚΟΠΗΣΗ ΩΜΟΥ
Οι καινοτομίες τόσο στην τεχνολογία των εμφυτευμάτων, όσο και στην εξέλιξη της αρθροσκόπησης, μας δίνει τη δυνατότητα να επεμβαίνουμε αναίμακτα πλέον στον ώμο, σε ένα μεγάλο φάσμα περιπτώσεων όπως η αστάθεια, η ρήξη των τενόντων, τα ασβεστώματα, ο παγωμένος ώμος, οι τενοντίτιδες κ.ά
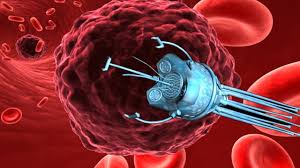
ΑΝΑΙΜΑΚΤΕΣ-ΒΙΟΛΟΓΙΚΕΣ ΘΕΡΑΠΕΙΕΣ
Η εξέλιξη της επιστήμης και ειδικά στον τομέα βιο-υλικών και εμφυτευμάτων έχει αλματώδη ανάπτυξη τα τελευταία χρόνια.
Συνέπεια αυτού είναι, να εφαρμόζονται ευρέως πλέον , στη κλινική πράξη, θεραπείες απλές, χωρίς τομές, με μία μόνο ένεση, [σε επίπεδο εξωτερικού ιατρείου] που στοχεύουν στην ανάπλαση ή την επούλωση χόνδρινων ή τενόντιων βλαβών.
Γεώργιος Α. Μπαμπαλής

Dr.Χρήστος Γιαννακόπουλος

Σδράκας Βασίλειος

Αγγέλης Κων/νος Αναισθησιολόγος

Νέλλα Παπαγιαννάκη

Μαρία Κάρδαρη

Ελένη Χοτζίδου
Μαριλίνα Νάνου
Διατροφολόγος
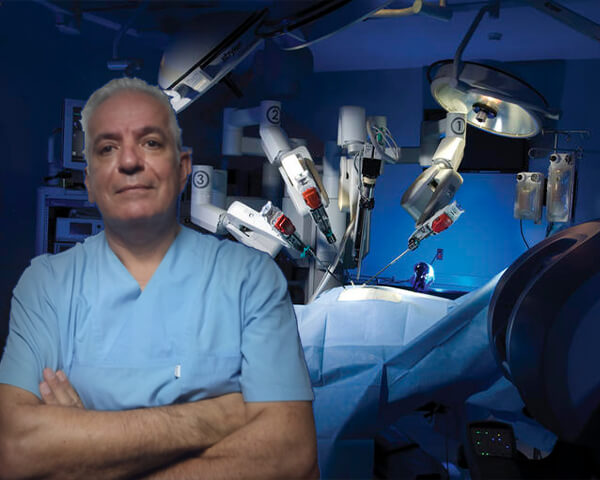
H IAΤΡΙΚΗ ΟΜΑΔΑ
Η έννοια της ιατρικής ομάδας, αποσκοπεί στην λεπτομερή, ακριβή και ενδεδειγμένη θεραπεία με σκοπό τα πολύ υψηλά ποσοστά αποτελεσματικότητας. Αυτό το επιτυγχάνουμε χρόνια τώρα, με γνώμονα την αποκατάσταση κάθε ασθενούς που θα αναλάβουμε.